Skipping pluripotency 'detour,' Max Planck researcher Schoeler again takes lead in stem cell research
Thursday, 22 March 2012
Breaking new ground, scientists at the Max Planck Institute for Molecular Biomedicine in Münster, Germany, have succeeded in obtaining somatic stem cells from fully differentiated somatic cells. Stem cell researcher Hans Schöler and his team took skin cells from mice and, using a unique combination of growth factors while ensuring appropriate culturing conditions, have managed to induce the cells' differentiation into neuronal somatic stem cells.
 |
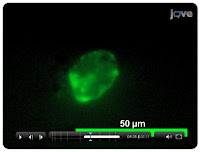
This is an immunofluorescence microscopy
image of the induced neural stem cells
(iNSCs) using antibodies against two neural
stem cell markers SSEA1 (red colour) and
Olig2 (green colour). Credit: MPI for
Molecular Biomedicine.
|
"Our research shows that reprogramming somatic cells does not require passing through a pluripotent stage," explains Schöler. "Thanks to this new approach, tissue regeneration is becoming a more streamlined - and safer - process."
Up until now, pluripotent stem cells were considered the 'be-all and end-all' of stem cell science. Historically, researchers have obtained these 'jack-of-all-trades' cells from fully differentiated somatic cells. Given the proper environmental cues, pluripotent stem cells are capable of differentiating into every type of cell in the body, but their pluripotency also holds certain disadvantages, which preclude their widespread application in medicine.
According to Schöler, "pluripotent stem cells exhibit such a high degree of plasticity that under the wrong circumstances they may form tumours instead of regenerating a tissue or an organ."
Schöler's somatic stem cells offer a way out of this dilemma: they are 'only' multipotent, which means that they cannot give rise to all cell types but merely to a select subset of them - in this case, a type of cell found in neural tissue - a property, which affords them an edge in terms of their therapeutic potential.
To allow them to interconvert somatic cells into somatic stem cells, the Max Planck researchers cleverly combined a number of different growth factors, proteins that guide cellular growth.
"One factor in particular, called Brn4, which had never been used before in this type of research, turned out to be a genuine 'captain' who very quickly and efficiently took command of his ship - the skin cell - guiding it in the right direction so that it could be converted into a neuronal somatic stem cell," explains Schöler. This interconversion turns out to be even more effective if the cells, stimulated by growth factors and exposed to just the right environmental conditions, divide more frequently.
"Gradually, the cells lose their molecular memory that they were once skin cells," explains Schöler. It seems that even after only a few cycles of cell division the newly produced neuronal somatic stem cells are practically indistinguishable from stem cells normally found in the tissue.
Schöler's findings suggest that these cells hold great long-term medical potential:
"The fact that these cells are multipotent dramatically reduces the risk of neoplasm formation, which means that in the not-too-distant future they could be used to regenerate tissues damaged or destroyed by disease or old age; until we get to that point, substantial research efforts will have to be made."
So far, insights are based on experiments using murine skin cells; the next steps now are to perform the same experiments using actual human cells. In addition, it is imperative that the stem cells' long-term behaviour is thoroughly characterized to determine whether they retain their stability over long periods of time.
"Our discoveries are a testament to the unparalleled degree of rigor of research conducted here at the Münster Institute," says Schöler.
"We should realize that this is our chance to be instrumental in helping shape the future of medicine."
At this point, the project is still in its initial, basic science stage although "through systematic, continued development in close collaboration with the pharmaceutical industry, the transition from the basic to the applied sciences could be hugely successful, for this as well as for other, related, future projects," emphasizes Schöler.
This, then, is the reason why a suitable infrastructure framework must be created now rather than later.
"The blueprints for this framework are all prepped and ready to go - all we need now are for the right political measures to be ratified to pave the way towards medical applicability."
Contact: Dr. Hans Schoeler
Reference:
Direct Reprogramming of Fibroblasts into Neural Stem Cells by Defined Factors
Han D.W., Tapia N., Hermann A., Hemmer K., Höing S., Araúzo-Bravo M.J., Zaehres H., Frank S., Moritz S., Greber B., Yang J.H., Lee H.T., Schwamborn J.C., Storch A., Schöler H.R.
Cell Stem Cell, 22 March 2012, 10.1016/j.stem.2012.02.021
.........