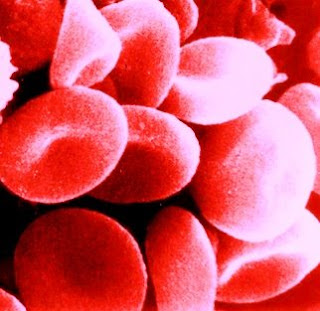
Blood Created by Identifying Earliest Stem Cells Friday, 29 August 2008 Johns Hopkins researchers have discovered the earliest form of human blood stem cells and deciphered the mechanism by which these embryonic stem cells replicate and grow. They also found a surprising biological marker that pinpoints these stem cells, which serve as the progenitors for red blood cells and lymphocytes. The biochemical marker, angiotensin-converting enzyme (ACE), is well known for its role in the regulation of blood pressure, blood vessel growth, and inflammation. ACE inhibitors are already widely used to treat hypertension and congestive heart failure. The findings are, the researchers say, likely to hold promise for developing new treatments for heart diseases, anaemia’s, leukaemia and other blood cancers, and autoimmune diseases because they show for the first time that ACE plays a fundamental role in the very early growth and development of human blood cells. "We figured out how to get the 'mother' of all blood stem cells with the right culture conditions," says Elias Zambidis, M.D., Ph.D., of the Institute of Cell Engineering at the Johns Hopkins University School of Medicine and the Division of Pediatric Oncology at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins. "There is real hope that in the future we can grow billions of blood cells at will to treat blood-related disorders, and just as critically if not more so, we've got ACE as a 'new' old marker to guide our work," Zambidis adds. Researchers did not expect ACE to have a role in blood stem cells, he notes, "but were very pleasantly surprised to discover it as a beacon for finding the earliest blood stem cells known, as well as new ways to find and manipulate this marker to make them grow." The team's findings, published Aug. 26 in the online edition of the journal Blood, explain that these earliest stem cells marked by ACE, called hemangioblasts, first arise normally in the developing human foetus, when a woman is three or four weeks pregnant. Hemangioblasts can now be derived in unlimited supply experimentally from cultured human embryonic stem cells, which are the origin of all cell types in the body. These hemangioblasts go on to become either blood cells or endothelial cells, which form the inner lining of the heart, veins and arteries, and lymph vessels. The research grew out of Zambidis' interest in understanding the complex biological processes of blood development and the transformation of embryonic stem cells into the various types of cells that make up the human body. Hemangioblasts make the body's earliest form of blood in the foetal yolk sac, which nourishes a fertilized egg, and later in the foetal liver and bone marrow. However, because human embryonic cells disappear early in gestation, their role in the early production of blood could not be studied in humans because scientists had no way to identify these human progenitor blood stems cells to follow their development. The scientists suspected they existed in humans, however, because they have been found in mice and zebra fish. To find the blood stem cell, Zambidis' team grew human embryonic stem cells in culture and fed them growth factors over 20 days. Each time the cell colonies expanded, the researchers sampled individual cells, searching for ones capable of making both endothelial and blood cells, the hallmark of hemangioblasts. They plucked the newly discovered hemangioblasts from culture dishes, grew them in conditions that Zambidis and his team developed to speed replication, and tested cells for their ability to make endothelial and blood cells. Cells capable of making endothelial cells and all the elements of blood (platelets, and white and red cells) were specifically marked with ACE on their outer surface. The researchers found not only that ACE was a marker for hemangioblasts, but also turning off the enzyme that helps guide the cells' replication and maturation into either blood or endothelial cells. By treating the hemangioblasts with losartan, an ACE pathway-blocking agent routinely used to treat high blood pressure, dramatically increased the rate of blood cell production. The next step, Zambidis adds, is to test this research in animal models and show that "we can make lots and lots of blood cells from human stem cells for transfusions, regenerate new vascular trees for heart diseases, as well as create test tube factories for making transplantable blood cells that treat diseases.” “We are very far from treatment but this is a big step," Zambidis caution. If the new technique of mass-producing progenitor blood cells is proven to work in humans, it would allow patients getting bone marrow transplants to have their own stem cells creating the blood they need, significantly reducing rejection risk. The research reported today used federally approved embryonic stem cell lines, but other related research by the team comes from non-approved lines. The study was supported by grants from the National Institutes of Health and the Maryland Stem Cell Research Fund. Reference: Expression of ACE (CD143) identifies and regulates primitive hemangioblasts derived from human pluripotent stem cells Elias T Zambidis, Tea Soon Park, Wayne Yu, Ada Tam, Michal Levine, Xuan Yuan, Marina Pryzhkova, and Bruno Peault Blood, online August 26, 2008; DOI 10.1182/blood-2008-03-144766 ......... ZenMaster
For more on stem cells and cloning, go to CellNEWS at http://cellnews-blog.blogspot.com/ and http://www.geocities.com/giantfideli/index.html