New Insight into Subtle Genomic Differences among Our Own Cells
Monday, 19 November 2012
Stanford University School of Medicine scientists have demonstrated, in a study conducted jointly with researchers at Yale University, that induced-pluripotent stem cells — the embryonic-stem-cell lookalikes whose discovery a few years ago won this year's Nobel Prize in medicine — are not as genetically unstable as was thought.
The new study, which will be published online Nov. 18 in Nature, showed that what seemed to be changes in iPS cells' genetic makeup — presumed to be inflicted either in the course of their generation from adult cells or during their propagation and maintenance in laboratory culture dishes — instead are often accurate reflections of existing but previously undetected genetic variations among the cells comprising our bodies.
That's good news for researchers hoping to use the cells to study disease or, someday, for regenerative medicine. But it raises the question of whether and to what extent we humans are really walking mosaics whose constituent cells differ genetically from one to the next in possibly significant respects, said Alexander Urban, PhD, assistant professor of psychiatry and behavioural sciences. Urban shared senior authorship of the study with bioinformatics professor Mark Gerstein, PhD, and neurobiology professor Flora Vaccarino, MD, both of Yale.
It's only a few years ago that human iPS cells started becoming available to researchers. These cells hold great promise because they act almost exactly like embryonic stem cells, which can be nudged to differentiate into virtually any of the body's roughly 200 different cell types. But iPS cells can be derived easily from a person's skin, alleviating numerous ethical concerns arising from the necessity of obtaining embryonic stem cells from fertilized eggs.
At least in principle, iPS cells' genetic makeup closely reflects that of the individual from whom they were derived. Today, "heart cells" derived from a heart patient's skin can be produced in a laboratory dish so scientists can learn more about that particular patient's condition and to screen drugs that might treat it. Tomorrow, perhaps, such cells could be administered to that patient to restore heart health without being perceived as foreign tissue by the patient's immune system, which would otherwise reject the implanted cells.
However, Urban said, several previous studies have raised worries regarding iPS cells' genomic stability. Whether it was the reprogramming procedure researchers use to convert ordinary adult cells into iPS cells or the culturing techniques employed to keep them alive and thriving afterward, something appeared to be inducing an upswing in these cells' manifestation of copy number variations, or CNVs — the disappearance or duplication of chunks of genetic material at specific locations along the vast stretches of DNA that coil to form the chromosomes residing in all human cells.
CNVs dot everybody's genomes. They occur naturally because of DNA-copying errors made during cell replication, and accumulate in our genomes over evolutionary time. The human genome, taken as a whole, is a DNA sequence consisting of four varieties of chemical units, strung together like beads on a roughly 3-billion-bead-long necklace. CNVs range in length from under 1,000 DNA units to several million. They account for up to several percent of the entire human genome, making them a major source of genetic differences between people.
But if either iPS cells' mode of generation or their subsequent maintenance in culture were promoting an increase in CNVs, it would seriously compromise these cells' utility in research and pose a fatal flaw to their use in regenerative medicine, said Urban.
"You would never want to introduce iPS cells into a patient thinking that these cells had the same genome as the rest of the patient's cells, when in fact they had undergone substantial genetic modifications you knew nothing about, much less their effects," said Urban. (Similar concerns apply to embryonic stem cells.)
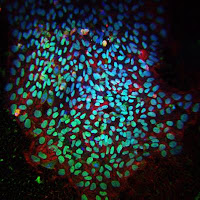
To see how serious a problem CNVs might pose for iPS cells' use, the collaborators performed tiny skin biopsies on seven volunteers and extracted cells called fibroblasts, which abound in skin and are amenable to cell culture in general and iPS cell generation in particular. From these, the team produced 20 separate iPS cell lines in culture. Using now-standard lab methods, the investigators determined, chemical unit by chemical unit, the full genomic sequence of the cells composing each new iPS cell line.
Urban and his colleagues, who had likewise assessed the fibroblasts from which the lines were derived, compared their genomic sequences with those of the newly generated iPS cells. The scientists were able to pinpoint numerous CNVs in the new cells that hadn't shown up in the fibroblasts. This raised the possibility that the rigors of reprogramming or life in a dish, or both, had led to new CNVs in the cells.
But the technique used to determine the full-length genome sequences of iPS cells and the "parental" fibroblasts from which they'd been spawned analyses not single cells but millions at a time. So a CNV residing in only a minority of cells within this mix could easily be missed, its signal swamped by the noise of the majority report.
Armed with knowledge of the precise locations along the genome where each of the "new" CNVs had popped up in their iPS cell lines, the scientists went back to the fibroblasts. This time, they used an analytical tool that, like a photocopying machine, can generate millions or billions of copies of a single section of DNA — provided that the specific DNA section is present to begin with. For each "new" CNV that had been unearthed in the iPS cells, a different version of this molecular copying machine was employed.
"Lo and behold, in many cases, this technique unearthed CNVs in the fibroblasts that were there all along but had been missed in the earlier, mass analysis," Urban said.
These CNVs had gone undetected because the fibroblasts in which they resided represented as little as a fraction of a percent of the fibroblasts in a biopsy sample. But any CNV in a fibroblast lucky enough to become the "parent" of the billions of iPS cells bearing its identical genomic "face" would now stick out like the proverbial sore thumb. Six out of the 20 different iPS cell lines sported at least one CNV unshared with the other lines, the investigators found. To the extent this reflects differences in parental fibroblasts, it means about 30 percent of the cells in human skin may harbour unique CNVs.
"This is a huge amount of cell-to-cell genetic variation," said Urban, who also participated in a recent study of human tissues conducted by the laboratory of Michael Snyder, PhD, professor and chair of genetics at Stanford. That study showed there can be distinct CNV patterns in kidney, pancreas and liver.
"Rather than monoliths, our bodies may be mosaics composed of cells whose genomes differ. What we do not know is whether or when these differences are dangerous, irrelevant or beneficial."
That may depend on the organ, said Urban.
"The more complicated something is, the more ways there are that something could go wrong with it. The brain is a particularly complicated organ. CNVs affecting cells in particular brain structures or areas could be playing a role in complex neurodevelopmental disorders such as schizophrenia and autism."
Urban intends to find out, he said.
Contact: Bruce Goldman
.........
For more on stem cells and cloning, go to CellNEWS at